Patient accumulators (deductibles, maximums, etc.)
Most health plans have limits on how much will be paid out in benefits and what a member's financial responsibility is. When claims are processed, the amounts applied to those limits are tracked in accumulators. This option displays an individual's accumulators so you can respond correctly to claim inquiries on deductibles, maximums, and other accumulated data.
Access a patient's accumulator history
- Choose one of the following options:
- While entering or processing a claim, use the star menu, from the
Patientoption, selectAccumulators. While in a claim, member, or dependent session, select
Accumulatorsfrom thePatientmenu.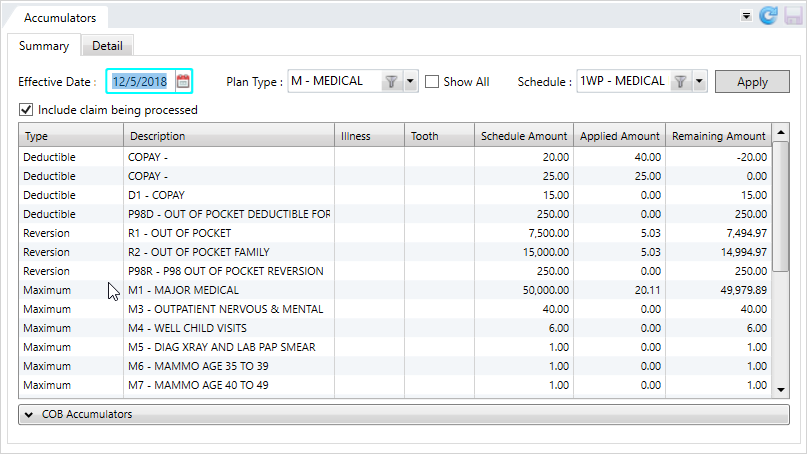
 Accumulators - Summary subtab field descriptions
Accumulators - Summary subtab field descriptionsField/Column Description The date the accumulator is in effect.
- From a claim session, displays the date of service from the first line on the claim.
- From a member or dependent session, if the individual has current eligibility, displays the current date. If the individual doesn't have current eligibility, then the most recent period of eligibility.
You can change the date to a past or future effective date.
- A future date in the current calendar year results in the same values as if using the current date.
- A future date in a subsequent calendar year displays accumulators for schedules that don't have termination dates. Applied values will be 0.
Plan Types
The claim benefit plan type (e.g. medical, dental, or vision). The first claim line determines the claim plan type.
- From a claim session, this displays the plan type from the claim.
You can select a different plan type from the list for the selected effective date.
- From a member or dependent session, this displays the default plan type setup. If there's no default plan type, then the first medical plan type on file displays.
Show All Check box to display all plan types—If the patient has more than one plan, select this option and choose the plans to include from the Plan Typeslist.Schedule
The claim schedule that defines the accumulators.
You can select a different schedule from the list for the selected effective date and plan type.
- From a claim session, this displays the schedule on the claim.
- From a member or dependent session, this displays:
- The PPO
 A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount. schedule associated with the benefit plan. If there's more than one PPO schedule, then the first one on file displays.
A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount. schedule associated with the benefit plan. If there's more than one PPO schedule, then the first one on file displays. - If there's no PPO schedule, then the default schedule for the benefit plan displays. If there's more than one default schedule for the benefit plan, then the first one on file displays.
- The PPO
Include claim being processed
Check box to indicate the accumulator table data reflects the current claim being processed.
If you accessed this tab via the
Actionmenu, you have the option of choosing to include the claim (see Action option.)Accumulators table Type
The accumulator type—Deductible, Reversion, Day Accumulator, or Maximum.
- COB
 A provision for determining benefits when a member has more than one benefit plan. accumulators display separately at the bottom of the tab. See Accumulator types for descriptions of each type.
A provision for determining benefits when a member has more than one benefit plan. accumulators display separately at the bottom of the tab. See Accumulator types for descriptions of each type.
Description
A description of the accumulator.
Illness
Amount applied to an illness limitation (deductible, count of days, etc.)
Tooth
The tooth number or group of teeth (can include a quadrant of the mouth), the dentist indicated the procedure was performed.
Schedule Amount
The amount specified in the schedule for the accumulator, (e.g. the deductible amount, maximum amount, or total number of days).
Applied Amount
- The total amount from all claims applied to the accumulator.
- For the Day Accumulator, the applied amount is the total number of days used.
Remaining Amount
The amount remaining for the accumulator. Calculated as:
Schedule Amount—Applied Amount.
- While entering or processing a claim, use the star menu, from the
- Select your filter options (see the table above for descriptions) and click
Apply.Show Allplans—If the patient has more than one plan, select this option and choose the plans to include.- A patient was previously eligible for a particular plan and has a claim paid under the plan during a period he wasn't eligible.
- Select a schedule for the claim where there was an applied claim. Depending on the selected date and the accumulator setup, any accumulator plans that had applied money towards that claim show the correct applied amounts.
- A patient wasn't previously eligible for a particular plan, but had a claim paid. A fund will only be available if there's a fund linked to the benefit plan. If there's no fund linked to the benefit plan, no accumulator information will display.
- A patient was previously eligible for a particular plan and has a claim paid under the plan during a period he wasn't eligible.
Include claim being processed—Clear or select to include the current claim in the accumulator totals.
- The Summary tab displays all eligible and ineligible accumulators for the selected effective date, plan type, and schedule.
Find claims associated to an accumulator
- To see the claims applied to an accumulator, double-click the accumulator in the Summary table.
-
The
Detailtab displays the claims (and the detail) associated with the selected accumulator.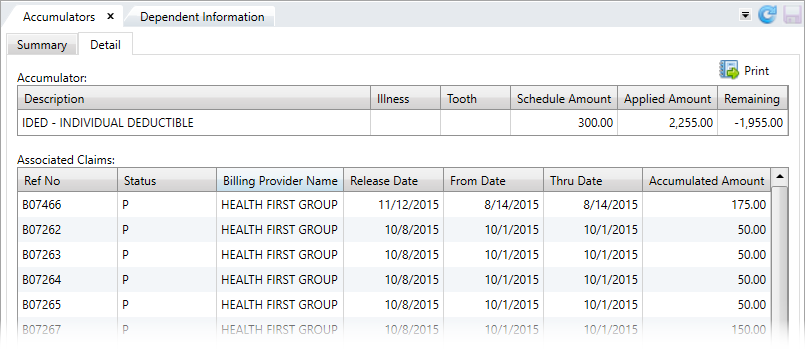
 Accumulators - Detail subtab field descriptions
Hint: Click
Accumulators - Detail subtab field descriptions
Hint: Click at the top right of the table to print the Claims History Report, containing the claims associated with the selected accumulator.
at the top right of the table to print the Claims History Report, containing the claims associated with the selected accumulator. Field Accumulator Type Description Accumulator: Description User-defined accumulator code followed by the description.
- This can be a Deductible, Maximum, Reversion, Day, or COB Accumulator. See Accumulator types
Illness Amount applied to an illness limitation (deductible, count of days, etc.) Tooth The tooth number or group of teeth (can include a quadrant of the mouth), the dentist indicated the procedure was performed.
Schedule Amount The accumulator amount defined in the schedule. Applied Amount The amount applied to the defined accumulator.
Remaining The remaining accumulator amount. Associated Claims: Ref No
All Types
The reference number for the claim.
Status
All Types
The status of the claim. See Claim statuses for descriptions.
Billing Provider Name
All Types
The individual or organization that issued the bill for the services listed on the claim.
Release Date
All Types
The date the claim was released. The release date doesn't indicate the claim was paid, but rather when the claim became available to be picked up in a check run.
From Date
Deductibles, Maximums, Reversions, and COB
The start date for the service provided.
Thru Date
Deductibles, Maximums, and Reversions
The end date for the service provided.
Accumulated Amount
Deductibles, Maximums, and Reversions
The claim amount applied to the accumulator. The
Applied Amountincludes all paid and released accumulated amounts from the associated claims in the table.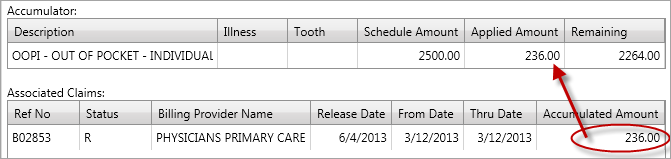
Date Days
The date the benefit was used.
Days Days
The day number the benefit was used (e.g. day 1, day 2, day 3, etc.).
Rev Le Days
The reversion level. The number of days at which a certain coinsurance amount applies. After this level, the next level takes effect and a different coinsurance amount.
- For example, days 1-4 fall into the reversion level of 1-4 and are paid out at 70%. Day 5 falls into a different level.
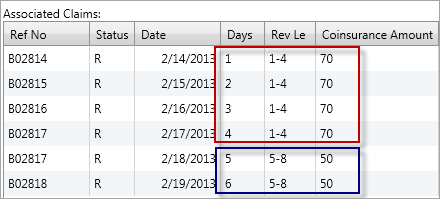
Coinsurance Amount Days
The coinsurance rate applied to the claim (e.g. 70 is 70%).
Bank Amount
COB
The coordination of benefits savings amount.
OOP Amount
COB
The out of pocket amount the patient owes.