Add, update, or delete coordination of benefits information
When members and dependents have multiple insurance plans, you need to make sure they're making payments from the correct plans. Managing multiple plans under a single member or dependent is known as coordination of benefits (COB![]() A provision for determining benefits when a member has more than one benefit plan.). See Coordination of benefits (COB) for more detailed information on COB plans.
A provision for determining benefits when a member has more than one benefit plan.). See Coordination of benefits (COB) for more detailed information on COB plans.
If you have a claim reference number, a member or dependent name or number, or you received a claim with new or updated COB information, use the Coordination of Benefits tab to view, add, update, or delete information.
- Search and open the claim, member, or dependent.
- From either the
PatientorClaimsmenu selectCoordination of Benefits.
Add a covered dependent for coordination of benefits
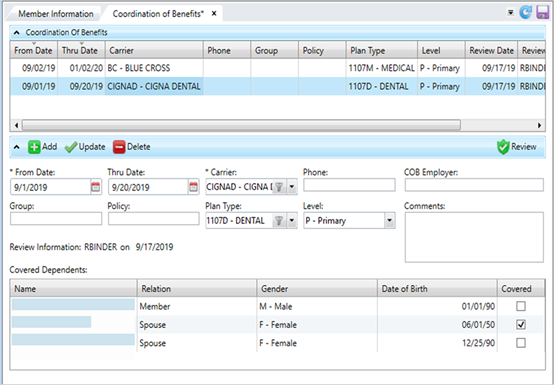
- On the Coordination of Benefits tab, click
 below the table.
below the table. - Update the insurance information and select the coverage from and thru dates.
- Select the check box for each individual that has coverage in the
Covered Dependentstable. -
Click
 to apply your changes.
to apply your changes. -
Click
 to save.
to save.
Update a COB entry
- Select the row to update.
- Make changes to the COB fields as necessary.
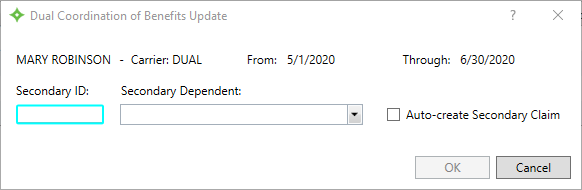
- If you’re offering employer-sponsored health benefits in your workforce, an employee of yours may qualify for what is called “dual insurance coverage” if her/his spouse is also receiving benefits from their respective employer (note: a child may also have dual insurance coverage if covered by both parents’ plans).
In such cases, the plan with the oldest policy holder is designated the “primary plan”, while the other is designated the “secondary” plan. The insurance carrier makes this designation, and it isn't selected by the employee making the claim. If needed, update any
 dependents covered under the same insurance (dual COB).
dependents covered under the same insurance (dual COB).
- If you’re offering employer-sponsored health benefits in your workforce, an employee of yours may qualify for what is called “dual insurance coverage” if her/his spouse is also receiving benefits from their respective employer (note: a child may also have dual insurance coverage if covered by both parents’ plans).
In such cases, the plan with the oldest policy holder is designated the “primary plan”, while the other is designated the “secondary” plan. The insurance carrier makes this designation, and it isn't selected by the employee making the claim. If needed, update any
- Click
 to apply your changes. The review date and operator name update.
to apply your changes. The review date and operator name update. -
Click
 to save.
to save.
* indicates a required field
| Field | Description |
|---|---|
| From Date* | The date of the other insurance coverage is in effect. Click |
| Thru Date |
The termination date of the other insurance coverage. |
| Carrier* | The organization that issued the insurance policy. Select a carrier from the list. |
| Phone | The carrier's phone number. Enter any alphanumeric or non-alphanumeric characters. |
| COB Employer | The employer associated with the benefit plan offering. This is a free-form text field to show the employer, but there is no validation on spelling or verification the employer is in the system. This information won’t display anywhere else. |
| Comments | Additional information associated with the insurance coverage. Any comment text longer than 30 characters will wrap and show in the text box. |
| Group | The group or employer name. Enter any alphanumeric or non-alphanumeric characters. |
| Policy | The policy number for the healthcare coverage. Enter any alphanumeric or non-alphanumeric characters. |
| Plan Type | The claim benefit plan type (e.g. medical, dental or vision). |
| Level |
The insurance plan order to pay the claim. The primary health insurance is the plan that pays the claim first, as if it were the only source of health coverage. Then, the secondary insurance plan picks up the cost left over after the primary plan has paid the claim.
|
| Covered Dependents |
The table lists each member of the family.
Dual COB
|
| Review Information |
Text that shows and the date and the operator ID of the person who last reviewed (clicked |
Delete a COB entry
- Select the row to delete.
-
Click
 to delete the row from the table.
to delete the row from the table. -
Click
 to save.
to save.