Verify a coordination of benefits (COB) claim
While processing or entering a claim, if a prepaid amount is entered or changed during the save process a coordination of benefits verification runs. You'll need to review the COB information before you can proceed.
If you're reviewing the COB because of a pend code, click the Claim session tab to return to the claim and resolve the pend.
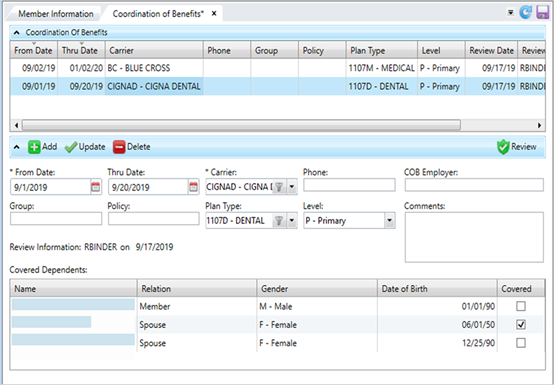
* indicates a required field
| Field | Description |
|---|---|
| From Date* | The date of the other insurance coverage is in effect. Click |
| Thru Date |
The termination date of the other insurance coverage. |
| Carrier* | The organization that issued the insurance policy. Select a carrier from the list. |
| Phone | The carrier's phone number. Enter any alphanumeric or non-alphanumeric characters. |
| COB Employer | The employer associated with the benefit plan offering. This is a free-form text field to show the employer, but there is no validation on spelling or verification the employer is in the system. This information won’t display anywhere else. |
| Comments | Additional information associated with the insurance coverage. Any comment text longer than 30 characters will wrap and show in the text box. |
| Group | The group or employer name. Enter any alphanumeric or non-alphanumeric characters. |
| Policy | The policy number for the healthcare coverage. Enter any alphanumeric or non-alphanumeric characters. |
| Plan Type | The claim benefit plan type (e.g. medical, dental or vision). |
| Level |
The insurance plan order to pay the claim. The primary health insurance is the plan that pays the claim first, as if it were the only source of health coverage. Then, the secondary insurance plan picks up the cost left over after the primary plan has paid the claim.
|
| Covered Dependents |
The table lists each member of the family.
Dual COB
|
| Review Information |
Text that shows and the date and the operator ID of the person who last reviewed (clicked |
- Verify that the Coordination of Benefits information is correct according to your office's operating procedures.
- Click
 to update the
to update the Review Informationdate and operator ID. -
Click
 to apply the update.
to apply the update. - After verifying the coverages, go back to the claim and resolve the edit by clicking the next edit arrow or use the
F9key.