Review an individual's COB
You can review an individual's COB![]() A provision for determining benefits when a member has more than one benefit plan. information periodically to ensure it is correct and up-to-date, for example:
A provision for determining benefits when a member has more than one benefit plan. information periodically to ensure it is correct and up-to-date, for example:
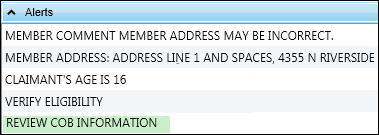
- You open a claim and it has an alert to review COB information.
- Search and open the claim.
-
On the
Patientmenu, selectCoordination of Benefits.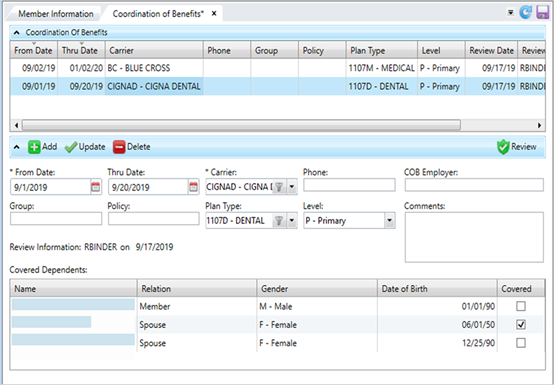
- Select the row in the Coordination of Benefits table to review. If you received information from the individual, you can verify the information against the file. Choose one of the following:
If all the information is correct, click
 once you have verified the information.
once you have verified the information.or
- If the information on file is incorrect, make changes and click
 . See Add, update, or delete coordination of benefits information.
. See Add, update, or delete coordination of benefits information.  COB Field Descriptions
COB Field Descriptions* indicates a required field
Field Description From Date* The date of the other insurance coverage is in effect. Click
 and select a date or enter a date in
and select a date or enter a date in MM/DD/YYYYformat.Thru Date The termination date of the other insurance coverage.
Carrier* The organization that issued the insurance policy. Select a carrier from the list. Phone The carrier's phone number. Enter any alphanumeric or non-alphanumeric characters. COB Employer The employer associated with the benefit plan offering. This is a free-form text field to show the employer, but there is no validation on spelling or verification the employer is in the system. This information won’t display anywhere else. Comments Additional information associated with the insurance coverage. Any comment text longer than 30 characters will wrap and show in the text box. Group The group or employer name. Enter any alphanumeric or non-alphanumeric characters. Policy The policy number for the healthcare coverage. Enter any alphanumeric or non-alphanumeric characters. Plan Type The claim benefit plan type (e.g. medical, dental or vision). Level The insurance plan order to pay the claim. The primary health insurance is the plan that pays the claim first, as if it were the only source of health coverage. Then, the secondary insurance plan picks up the cost left over after the primary plan has paid the claim.
P—PrimaryS—SecondaryT—Tertiary
Covered Dependents The table lists each member of the family.
Name—The name of the individual.Relation—The relationship to the dependent (e.g. Member, Spouse, Child).Gender—The individual's sex (M—male, F—female or U—unknown). Select unknown if you don't know the sex. Update the record once you do know.Date of Birth—The individual's birth date.Covered—A check mark indicates the individual is covered by this insurance policy. You must select at least one individual.
Dual COB
 Primary and secondary coverage claims that are processed by the same fund office. fields (displays based on system configuration)
Primary and secondary coverage claims that are processed by the same fund office. fields (displays based on system configuration)Second ID—The policy SSN for the secondary claim. If your system is configured for masking and is turned on, it will be masked.Sec Depno—The dependent number of the secondary covered dependent. When you enter the SSN into theSecond IDfield, theSec Depnodefaults to that dependent's number.Auto-create—Override automatic creation for a secondary claim. The claim will need to be processed manually
Review Information Text that shows and the date and the operator ID of the person who last reviewed (clicked
 ), updated, or deleted the COB information.
), updated, or deleted the COB information.The review date and operator update.
-
Click
 to save.
to save.
Resolve a held or pended claim
If you're reviewing the COB because of a pend code, click the Claim session tab to return to the claim and resolve the pend.