Claimant Audit
Use the Claimant Audit screen to specify the criteria used to select claims of individuals or all family members for audit. You can create more than one audit criteria with overlapping from and thru dates if needed.
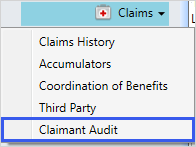
Access Claimant Audit
There are a few ways to access Claimant Audit from a member, dependent, or claim:
- Search for and open a member or dependent.
- Select
Claims, and then selectClaimant Audit.
OR
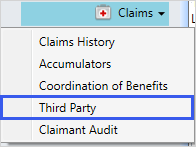
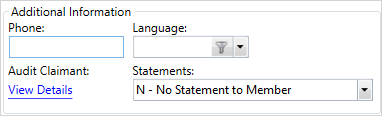
- Search for and open a member or dependent.
- Select
Claims, and then selectThird Party. - From
Audit Claimant, selectView Details.
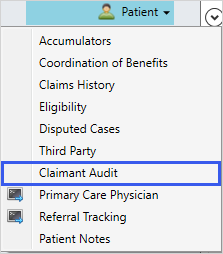
OR
- Search for and open a claim.
- Select
Patient, and then selectClaimant Audit.
The Claimant Audit screen displays the audit criteria.
| Field | Description |
|---|---|
| From Date* | The from date for the audit criteria. This prompt is required when adding or updating criteria (this prompt considers the date of service on each claim line). |
| Through Date* | The through date for the audit criteria. This prompt is required when adding or updating criteria (this prompt considers the date of service on each claim line). |
| Audit Type* |
Determines if claims for this member or dependent will be selected for automatic audit. (See Process Overview, Held Claims.) This prompt is required when adding or updating criteria:
|
| Comment | Enter an optional comment about the audit criteria. You can enter up to 36 characters. |
| Inactive |
Select the check box if the audit criteria is inactive. |
| Modified By | The name of the operator who last modified the criteria. |
| Modified When | The date and time the operator last modified the criteria. |
| Criteria | Includes a check mark |
| Fund | The fund |
| Group | Group for which the claim was processed. |
|
Plan Type |
The claim benefit plan type (e.g. medical, dental, or vision). The first claim line determines the claim plan type. |
|
Operator |
User ID of the individual who entered the information. |
| Subgroup | Subgroup |
|
Plan |
Plan for which the claim was processed. |
| PPO | Preferred Provider Organization (PPO) code used in paying the claim. |
| Schedule | The schedule for the criteria. |
| Coverage | The coverage code identifies who is covered by a benefit plan type, for example, individual or family. |
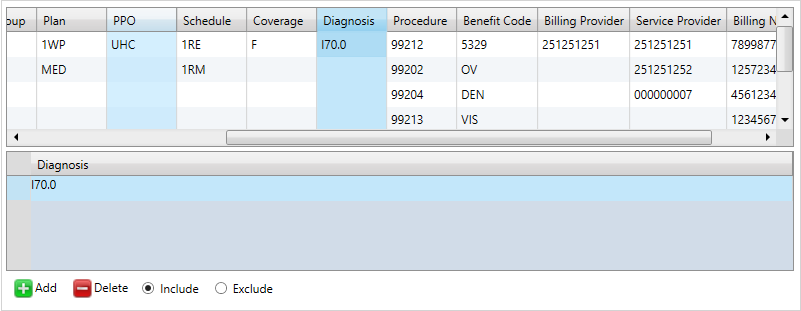
| Diagnosis | The ICD diagnosis code for the claim. |
| Procedure |
A code that identifies a specific service performed by a service provider. Note: There is a standard set of Procedure codes but your office might use other codes such as revenue or internal codes for your Procedure codes. |
| Benefit Code |
The benefit code representing a benefit or service covered in the Summary Plan Description document (e.g. eye exam, emergency outpatient care or an office medical visit). |
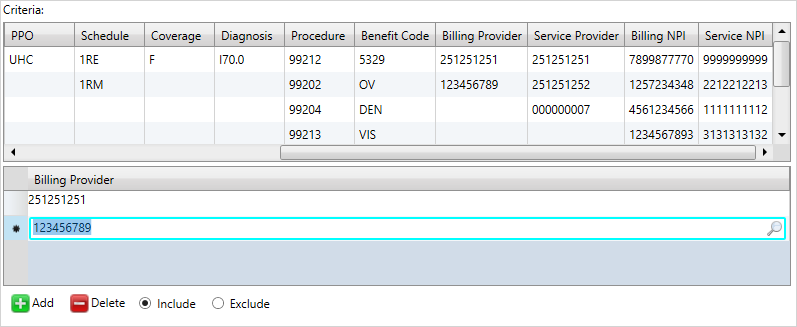
| Billing Provider | The individual or organization that issued the bill for the services listed on the claim. |
| Service Provider |
The service provider's ID number. |
| Billing NPI | The service provider’s National Provider Identifier (NPI). This is a 10-digit ID assigned to the provider by the National Plan and Provider Enumeration System (NPPES). It is possible for service providers under one billing provider to have the same NPI. For example, groups or organizations with multiple subparts could share the same NPI. |
| Service NPI | A unique identifier issued by the National Plan and Provider Enumeration System (NPPES) to all health care service providers who want to send or receive HIPAA transactions. |
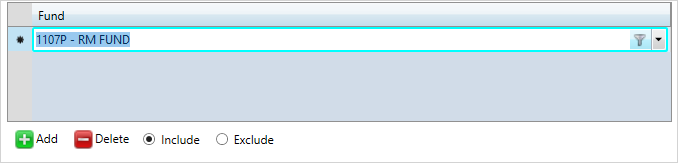
Add audit criteria
- From the
Claimant Audit Infotable, select to add audit criteria.
to add audit criteria. - Select the
From Date,Through Date, andAudit Type. - Enter an optional
Comment. - If the criteria is inactive, select the
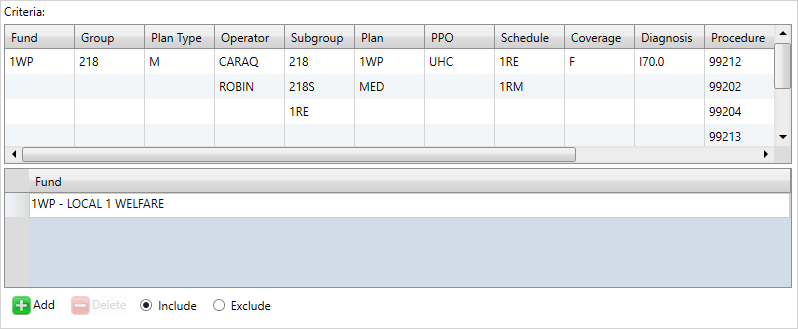
Inactivecheck box. - Choose the criteria used to select claims of individuals or all family members for audit as needed. If you don't enter any criteria, all claims will be audited. At the
Criteriatable, clickFundin the table in the upper table. - Select
 to specify a fund to include in the lower table. Choose a fund from the dropdown list.
to specify a fund to include in the lower table. Choose a fund from the dropdown list. - Click
Includeto include the fund or clickExcludeto exclude it. -
Select another criteria to add from the table, for example,
Group. TheFundfield updates. - Complete the above steps to select a
Group,Plan Type,Operator,Subgroup,Plan,PPO,Schedule, andCoverage. - For the
Diagnosis,Procedure,Service Provider,Billing NPI, andService NPIfields, click a row in the upper table and enter a value in the lower table. - For the
Benefit CodeandBilling Providerfields, click in the row in the upper table, and search for a value in the lower table. - If you need to delete any of the values, select the criteria from the row and press
 .
. - After creating the audit criteria, click
 .
. - Click
 to save.
to save.
Update audit criteria
- From the
Claimant Audit Infotable, select the audit criteria to update. - Edit any of the information as necessary.
- Click
 .
. - Click
 to save.
to save.
Delete audit criteria
- From the
Claimant Audit Infotable, select the audit criteria to delete. - Click
 to delete the criteria.
to delete the criteria. - Click
 to save.
to save.