A billing provider can be either a group of service providers or one service provider that is the same as the billing provider. The billing provider will receive payments for services provided by its service providers. The billing provider file is the basis for maintaining service providers as well as the means of issuing 1099's at the end of the year. It’s imperative that this information be carefully updated.
As billing providers are added, they are automatically created as service providers of themselves.
Before additional service providers are added, determine whether these providers will be added based on an actual individual ID number or based on system created incremental numbers.
- Using a provider's actual ID# will improve your ability to identify service providers and reference data.
- Service providers can be added through Add/Update Provider or during Claim Entry. Decide which method is best for your site and develop a process and train the appropriate individuals. See Add billing and service providers.
- Be sure they are clear on PPO and Discount arrangements and how they are maintained on the service provider level. Also remember to set up the provider as a PCP
 A physician who serves as a group member's primary contact within the health plan. In a managed care plan, the primary care physician provides basic medical services, coordinates and, if required by the plan, authorizes referrals to specialists and hospitals. if you're using Point of Service
A physician who serves as a group member's primary contact within the health plan. In a managed care plan, the primary care physician provides basic medical services, coordinates and, if required by the plan, authorizes referrals to specialists and hospitals. if you're using Point of Service A Point of Service (POS) plan is an "HMO/PPO" hybrid; sometimes referred to as an "open-ended" HMO when offered by an HMO. POS plans resemble HMOs for in-network services. Services received outside of the network are usually reimbursed in a manner similar to conventional indemnity plans (e.g., provider reimbursement based on a fee schedule or usual, customary and reasonable charges)./referral tracking
A Point of Service (POS) plan is an "HMO/PPO" hybrid; sometimes referred to as an "open-ended" HMO when offered by an HMO. POS plans resemble HMOs for in-network services. Services received outside of the network are usually reimbursed in a manner similar to conventional indemnity plans (e.g., provider reimbursement based on a fee schedule or usual, customary and reasonable charges)./referral tracking Tracking process that allows administrators to manage health care costs with a Primary Care Physician is the "gatekeeper" for participants' health care needs..
Tracking process that allows administrators to manage health care costs with a Primary Care Physician is the "gatekeeper" for participants' health care needs..
- Be sure they are clear on PPO and Discount arrangements and how they are maintained on the service provider level. Also remember to set up the provider as a PCP
Billing Provider Information has three subtabs—Demographics, Tax Information, and Billing Provider PPO Matching.
Demographics tab
The Demographics tab displays the billing provider's name and alternate billing names along with some billing provider options, such as if members receive an EOB when the billing provider is paid.
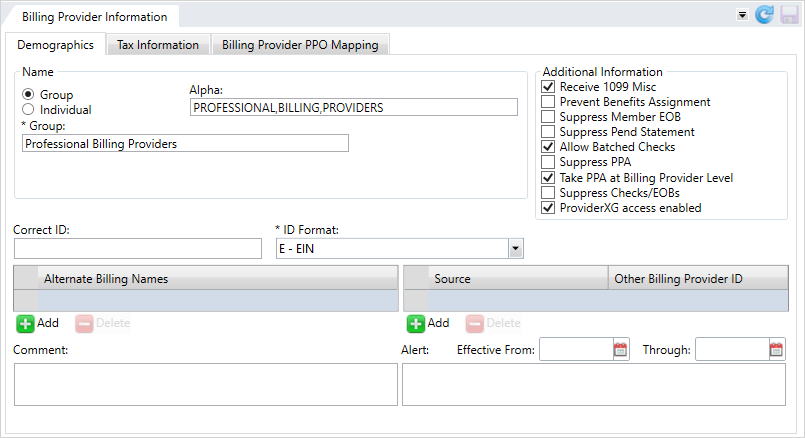
* indicates a required field
| Name | |
| Group/Individual |
Select either |
| Alpha |
Auto-updated, read-only field based on the group or individual information entered, used to sort the provider's name in reference lists. |
| Group | The provider group's name. |
|
Individual |
When the provider isn't in a group these fields apply.
|
| Additional Information | |
|
Receive 1099 Misc |
Indicates the 1099-MISC form will be sent to the billing provider when it's issued. |
|
Prevent Benefits Assignment |
Prevent operators from assigning services and benefits to the billing provider. |
|
Suppress Member EOB |
Prevent generating member EOBs |
|
Suppress Pend Statement |
Prevent a pend statement being generated for the billing provider. |
|
Allow Batched Checks |
Indicates that batch multiple claims payable to the billing provider are on one check. |
| Suppress PPA |
Indicates that the PPA window won't display in claims entry or claims processing when the associated service provider is on the claim.
This field won’t display for the first service provider associated with this billing provider. If an operator isn't allowed to take PPA (security settings), the PPA window will be suppressed. If the provider or member has a PPA, pend code P28 will be applied to the claim so that an operator who has the ability to determine whether to take PPA or not can complete the claim. Note: Contact your basys representative to set or change SAC (System Administration Control) settings. Don't change SACs without first consulting basys as changing them can affect other functions and global system settings.
|
| Take PPA at Billing Provider Level |
Note: Contact your basys representative to set or change SAC (System Administration Control) settings. Don't change SACs without first consulting basys as changing them can affect other functions and global system settings.
|
| Suppress Checks/EOBs | Indicates that checks and EOBs are suppressed for the billing provider. |
| ProviderXG access enabled |
Enables user access to the ProviderXG portal. You must select this check box to let Provider contacts access ProviderXG (see Add, update, or delete a provider contact). Note: If you restrict access to ProviderXG and then enable access again, the contacts previously set up to use the portal on the billing provider's Contacts screen keep their account credentials.
|
|
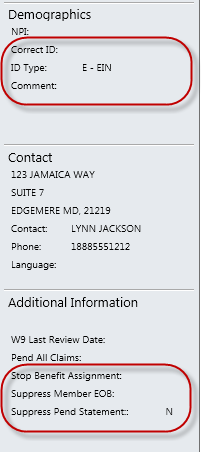
Correct ID |
The ID to use for this billing provider. A billing provider with this ID must already be in the system.
|
|
ID Format* |
The provider ID format.
|
|
Alternate Billing Names |
Names other than the billing provider or service provider associated with this billing provider. |
|
Source/Other Billing Provider ID |
Other billing provider identifiers along with the source of the ID.
|
|
Comment |
Additional information associated with the provider. Include information that will help other users quickly respond to inquiries about the billing provider. The comment can be up to 50 characters long. |
|
Effective From Effective Through |
Start and end dates for provider alert messages. Click MM/DD/YYYY format. Alerts with effective dates only show on a claim when they are within the effective date range. |
|
Alert |
Important or critical information about the provider. The alert can be up to 150 characters long.
|
Key information from this tab displays on the Provider session Demographics and Additional Information data tiles.
Tax Information tab
The Tax Information tab shows W-9 tax information for the billing provider. See Update W-9 information.
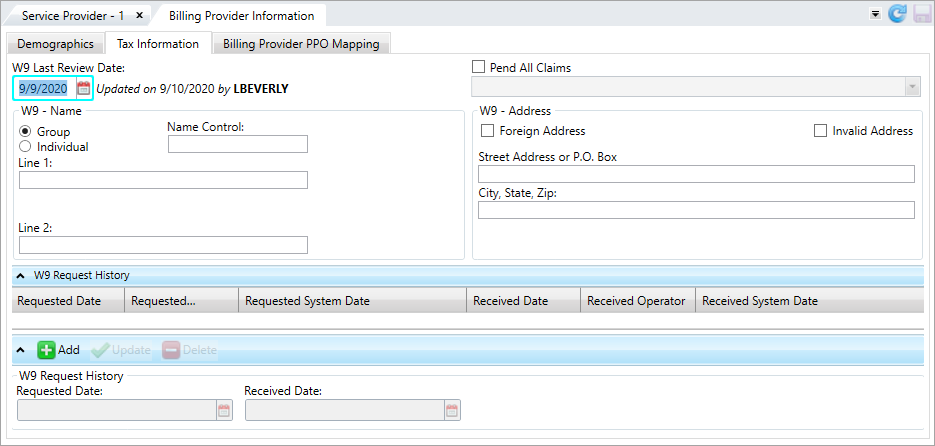
* indicates a required field
W9 request history table fields
Billing Provider PPO Mapping tab
Use the PPO Mapping tab to match billing providers with a PPO![]() A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount. based on specific criteria. See Map provider PPOs for more information.
A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount. based on specific criteria. See Map provider PPOs for more information.
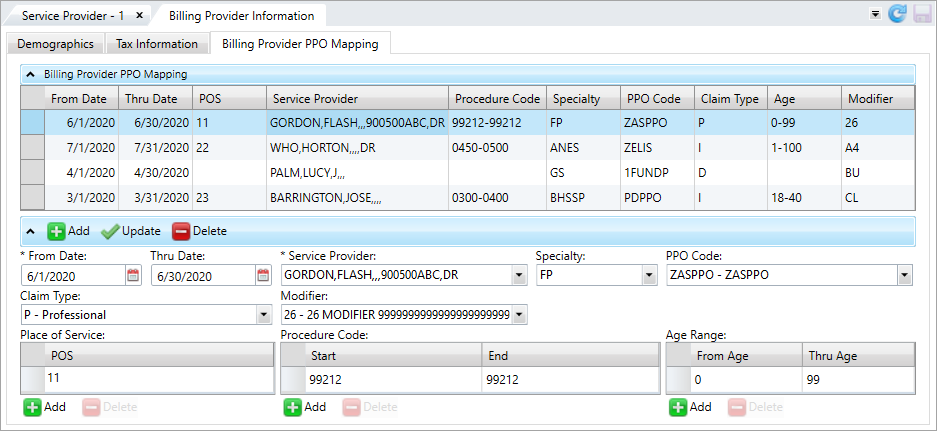
* indicates a required field
| Field | Description |
|---|---|
| From Date* | The first date the PPO match is active. |
| Thru Date | The PPO term date, or the PPO match's end date. |
| Service Provider* |
The service provider
|
| Unique ID | The provider's unique ID with the PPO. If a claim is submitted with this unique ID, it's matched to the related service provider. |
| PPO |
The PPO |
| Claim Type |
The claim type to map.
|
| Modifier | The modifier |
| Specialty | The service provider's specialty to map (includes all specialties listed in the system). |
| POS (Place of Service) | The place(s) of service to map. |
| Procedure Code (Range) | The procedure code |
| Age (Range) | The patient age range to map. If a patient’s age is outside of this range, this provider will not be used for the matching process. |