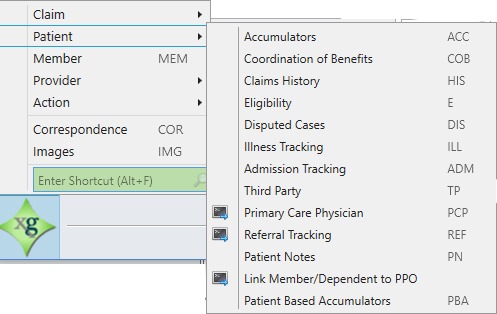
From the star menu patient option, access:
Accumulators ACC
Access Accumulators to view the patient's accumulator totals (deductibles, maximums, etc.). When you choose this option while processing a claim a message displays asking if you want to Include the current claim in the accumulator totals. See Patient accumulators (deductibles, maximums, etc.).
- To include the current claim in the accumulator summary totals click
YES. - To view the accumulator totals without including the current claim, click
No.
Coordination of Benefits COB
Use COB to record and track Medicare and other insurance information to ensure your office correctly pays out claims. Access this function from the Star menu during claims processing or claims entry, or from the Claims menu in either a Member or Dependent session. See Coordination of benefits (COB).
Claims History HIS
The Claims History tab shows a summary of all claims for an individual. See Claims history.
Eligibility E
The Eligibility tab provides complete eligibility for benefits, (medical, dental, and vision). This includes eligibility awarded to individuals from contributions, premium billing, direct pay, COBRA, and eligibility overrides. See Eligibility.
Disputed Cases DIS
This option allows you to track disputes. Disagreements often arise about the amount due on a bill, the amount the insurance company paid on a claim, or the nonpayment of a claim. See Disputed cases.
IllnessTracking ILL
The Illness tracking tab is used to track claims related to a certain health event. Depending on the procedure involved, illness tracking information can automatically become a choice in the Links workspace Linked Illness for Line 1 list (see the Claims Lines workspace field descriptions in Lines—The Lines workspace is tailored to the specific professional, institutional, and dental forms and contains the necessary values for each (Professional CMS 1500 Claim Form, Institutional CMS 1450/UB-04 Form, and Dental – ADA Form). See Diagnosis codes for the claim. Each diagnosis code has a corresponding diagnosis pointer (with the exception of Institutional)—a single alpha character preceding its corresponding diagnosis code, for example, A: 480. . ). See Illness tracking.
Admissions Tracking ADM
Access the Admissions Tracking tab to track claims related to a hospital admission. Depending on the procedure involved, admissions tracking information automatically becomes a choice in the Links workspace Linked Illness for Line 1 list (see the Claims Lines workspace field descriptions in Lines—The Lines workspace is tailored to the specific professional, institutional, and dental forms and contains the necessary values for each (Professional CMS 1500 Claim Form, Institutional CMS 1450/UB-04 Form, and Dental – ADA Form). See Diagnosis codes for the claim. Each diagnosis code has a corresponding diagnosis pointer (with the exception of Institutional)—a single alpha character preceding its corresponding diagnosis code, for example, A: 480. . ). See Admissions tracking.
Third Party TP
The Third Party option lets you view and enter Third Party information. Use this option when the check should be sent to a party other than the Billing Provider or the Member. Third Party uses an ID number and is used when the payment is submitted to a bank in the form of a direct deposit. See Third party overview.
Primary Care Physician PCP
The Primary Care Physician (PCP) is the member or dependent's primary source of medical attention—the "gatekeeper" for health services for the person. Use this option to view links to the primary care physician at the dependent level. For detailed information on Primary Care Physician, search for "PCP" in the ClaimsXG User Manual.
Referral Tracking REF
Use the Referral Tracking option to add, update, and delete referrals, as well as to view claims associated with the referral. For detailed information on Referral Tracking, search for "<REF>Referrals" in the ClaimsXG User Manual.
Patient Notes PN
The Patient Notes tab is where you can add, update, and delete information about the patient that could display to operators during processing (depending on your system settings). See Add, update, or delete patient notes.
Link a Member/Dependent to PPO
Use this option if a plan has multiple PPO![]() A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount. options and requires that the member selects a PPO. See Link a member or dependent to PPO.
A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount. options and requires that the member selects a PPO. See Link a member or dependent to PPO.
Patient Based Accumulators PBA
Patient Based Accumulators are special accumulators approved on a case-by-case basis. You can add, update, and delete Patient Based Accumulator information on the Patient Based Accumulators subtab. On the Details subtab you can associate a schedule or benefit code with an accumulator. See Patient based accumulators (PBA).